What is anaplasmosis? Why you need to know about this tick-borne illness!
(This post may contain affiliate links. See the full affiliate disclosure here for more info.)
Maybe you’ve been asking, “What is anaplasmosis” and “How is anaplasmosis different from Lyme disease?”
Sometimes life takes the oddest of turns. I wrote a post this spring on preventing tick bites. The smallest section was on anaplasmosis in humans, a tick-borne illness.
Well, since then, I’ve had anaplasmosis, and it deserves much more than a few sentences.
What follows is my experience with anaplasmosis, some human granulocytic anaplasmosis facts, and answers to some frequently asked questions on anaplasmosis in humans.
What is anaplasmosis? Anaplasmosis symptoms
Are you wondering what it’s like to have anaplasmosis or think that you might have anaplasmosis?
For several days, I had a low-grade fever of lower than 101 °F. My most striking symptom was teeth-chattering chills. I don’t remember having those with fevers in the past. I did eat and drink fluids, but not enough, apparently (more on that later).
Times being what they are, by the second day, I decided that I had COVID. A rapid home test was negative. Another test the next day was also negative.
On the third day, I had plans to pick up a new puppy with my daughter. I planned to go since I was working under the assumption that I had a virus, but not COVID.
However, my chattering teeth made my daughter urge me to forgo the trip and get a drive-through rapid COVID polymerase chain reaction (PCR) test. That test was negative, too.
Now I was stuck. Thinking I might have the flu (although it’s not really flu season) or a urinary tract infection (despite the lack of urgency, frequency, burning, or other symptoms), I went to an urgent care clinic.
I had seen no signs of a recent tick bite, so a tick-borne illness wasn’t on my radar.
Trip to urgent care
Even though it wasn’t flu season, I had flu-like symptoms. The nurse at urgent care conducted all the usual vital sign tests, including a flu test, which was negative, and urinalysis. The urinalysis dipstick test revealed some protein and red and white blood cells, all of which can indicate a urinary tract infection.
She said that my symptoms indicated the need for more bloodwork, which could not be done there and urged me to go to the emergency room. I really did not feel like that was necessary.
However, when she handed me the yellow stickie with my urinalysis dipstick results, my eye caught “bili +,” indicating that bilirubin was found in my urine.
I knew that was a sign of a liver issue and didn’t protest when she said she was calling ahead to the ER to tell them I’d be coming soon.
Trip to the emergency room
I chose to go to the ER at a small local hospital, knowing that it was affiliated with the larger local teaching hospital nearby but also knowing that I wouldn’t sit for hours waiting to be seen. I was right, I was seen right away.
After taking the usual vital signs and clean-catch urine, an IV was started, and blood was collected for analysis. Nurses and a doctor took my medical history and focused on my fever, chills, and headache.
They asked if I had a rash anywhere (I did not) or had experienced a tick bite. I had not experienced anything I equated with a tick bite. Blood was drawn for blood tests to evaluate different systems (blood cells, liver and kidney functions, electrolyte levels, Lyme disease, and anaplasmosis).
They positioned the monitors behind the head of my bed where I could not see them, but my husband could. They attached a blood pressure cuff and programmed it to take my pressure every 15 minutes.
What I didn’t know at the time was that I had walked into the ER with a blood pressure of 70 over something (yikes). That is alarmingly low.
My low blood pressure was attributed to dehydration from the fever, and before it was over, I had received 5000 ml (5 liters!) of saline by IV. Interestingly, I never felt light-headed or had other effects from my low blood pressure.
Another doctor said it could be a physiologic consequence (of something) and not due to dehydration…but, regrettably, I forgot exactly what he said.
Admission to the hospital and the blood test results
Because my blood pressure was not improving very quickly and I needed continuous IV treatment, I was admitted to the hospital.
Shortly, my blood test results came back.
I had low white blood cells (3500/mm3. Normal is 4 – 9.5 mm3) and platelets (139,000/mm3. Normal is 145,000 to 357,000/m3) and elevated liver enzymes.
Aha! That might have been indicated by the positive urinary bilirubin at urgent care, although my serum bilirubin level was normal.
My liver enzymes were not astronomically elevated, but my alanine aminotransferase was 178 U/L (normal is 0 – 30 U/L), aspartate aminotransferase was 158 U/L (normal is 0 – 30 U/L), and my alkaline phosphatase was 138 U/L (normal is 35 – 105 U/L).
I also had a negative Lyme test (another tick-borne) disease but low magnesium and potassium levels. Some supplements to my IV solution quickly fixed those low levels.
Anaplasmosis diagnosis and anaplasmosis treatment
My doctor said that I was “the poster child” for someone with anaplasmosis. I had the signs and symptoms of anaplasmosis.
I was the right age (it’s more common in older people), I had fever and chills, and the lab results triad of decreased white blood cells and platelets and elevated liver enzymes.
I was started on oral doxycycline, that I would take twice a day for 10 days. I immediately lost my appetite.
I spent the night in the hospital and was only allowed to leave after I had received 5000 ml of saline and eaten something. In addition to the IV, I drank tons of fluids, all of which were measured coming and going.
The day after admission, my white cell count had dropped to 2.1/mm3, my platelets had dropped to 101/mm3, and my liver enzymes were somewhat lower but still elevated.
A few days later, the anaplasmosis test result came back positive. I was the 4th inpatient within the tiny hospital of fewer than 25 beds with anaplasmosis!
My recovery from anaplasmosis
After about 24 hours, the fevers stopped. But my appetite didn’t return until I stopped taking the doxycycline. It took a week for all the fluid I was given (and the 10 pounds I gained!) to leave my body.
Blood work done at a follow-up visit to my primary care physician a few days after admission showed that my white cell count and platelets had returned to normal—even though I was experiencing some random and new bruising.


My alkaline phosphatase level was now normal, but my alanine aminotransferase was 201 U/L (normal at this institution is 6 – 29 U/L), and my aspartate aminotransferase was 122 (10 – 35 U/L).
And I had not been drinking AT ALL, which can affect the results. I will have these checked in another 3 weeks.
It’s been more than 2 weeks, and I am still very tired. The random bruising has stopped, but I nap, literally SLEEP, for a couple of hours every afternoon.
I work to drink plenty of fluid every day and keep as active as possible.
The worst part is that I am afraid to spend time in the garden.
The first thing we did when I got home was to buy permethrin spray and find a pair of pants and a long-sleeved shirt that we dedicated to outdoor work. We put the clothes on hangers, hung them outdoors, and sprayed them with permethrin until they were wet.
I wear them outdoors when I enter grassy or garden areas. I wear socks that I pull up over the pant legs and spray my hat, boots, and exposed body parts with homemade tick repellent or tick repellents containing DEET.
I NEVER go out into the grass, even mowed grass, even just to walk the dog without my barnyard boots.
I consider myself lucky. I know someone who spent 2 weeks in the intensive care unit with anaplasmosis and another person who experienced many complications of anaplasmosis and lost 80 pounds.
Frequently asked questions about anaplasmosis
1. What ticks carry anaplasmosis?
Anaplasmosis is caused by the bite of an infected tick—a black-legged tick or deer tick (Ixodes scapularis) carrying the bacterium anaplasma phagocytophilum (a. phagocytophilum). These are very tiny ticks that are hard to spot.
They are widespread throughout the eastern United States and very concentrated in certain areas.
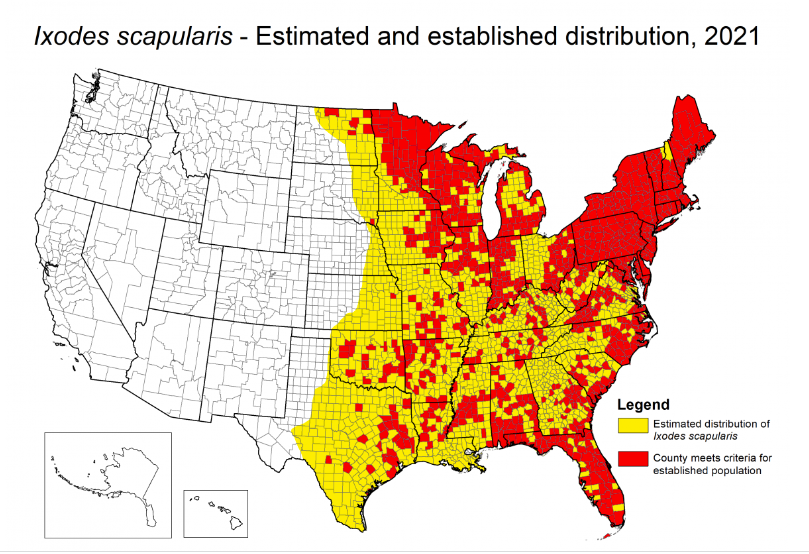
2. Where is anaplasmosis common?
Anaplasmosis is most common in two areas in the United States, the Midwest and New England.
3. What are the most common symptoms of anaplasmosis?
Anaplasmosis (and Lyme disease), which is also very common where I live, have some similar symptoms. They both show symptoms of an acute febrile illness, meaning fever.
The symptoms of anaplasmosis are fever, fatigue, headache, body and muscle aches, and sometimes, a rash. You may have a combination of symptoms or mild symptoms.
Lyme disease has similar symptoms but may also show a target-type rash around the bite.
4. I was bitten by a tick. Should I worry about anaplasmosis or other tick-borne infections?
Yes! If you have had a recent tick bite, first, look for the target rash that is characteristic of Lyme disease. If there is no rash, you can watch for the symptoms listed above or call your healthcare provider for advice right away.
Some doctors start their patients on doxycycline if a tick is discovered within 2 days of finding an embedded tick. Anaplasmosis can have life-threatening complications. Do not wait to seek treatment.
5. How is anaplasmosis diagnosed?
A blood test for anaplasmosis makes the definitive diagnosis. But it can be suspected by the symptoms of fever, fatigue, and rash and signs that include a low white blood cell count, low platelet count, and elevated serum liver enzymes.
Those findings are enough to strongly suspect anaplasmosis and initiate treatment with doxycycline even if no tick bite is found.
6. How is anaplasmosis treated?
Antibiotic treatment with doxycycline is the first-line treatment.
7. How long will I be sick with anaplasmosis?
In my experience, it took about 2 weeks before I felt better, even though the doxycycline treatment stopped the fevers in a day or so.
I am almost 3 weeks out from my hospitalization for anaplasmosis as I write this. My need to nap has decreased, my energy is increasing, and my fear of entering my garden is decreasing.
8. What can happen if anaplasmosis is not treated?
This is a very important question, as untreated anaplasmosis can result in severe illness. Unlike Lyme disease, some people, about 1%, die of an anaplasmosis infection.
People with untreated anaplasmosis might experience difficulty breathing, hemorrhage, renal failure, or neurological problems like convulsions and seizures.
These severe symptoms occur more often in immunocompromised people and people with other medical conditions than in normally healthy individuals.
9. Are there long-term effects of anaplasmosis in humans?
Another difference between Lyme disease and anaplasmosis is its long-term effects. Long-term effects, especially joint pain and fatigue, can be experienced by people who get Lyme disease, even if it is treated.
Such long-term effects have not (yet) been reported following successful anaplasmosis treatment. That is not to say, though, that serious complications can’t occur from the infection (see above) because they do and should never be discounted.
Take home messages on anaplasmosis
If you experience fever and chills with a negative COVID test, get checked by a physician as soon as possible, especially if you may have experienced a tick bite—even if you never identified a bite.
DO NOT WAIT BEFORE GETTING TREATMENT. Most severe complications occur in people who do not get prompt treatment or are compromised in some way due to their age or other medical problems.
One of the best ways to fight ticks is to kill ticks where you live by making tick tubes, treating your outdoor clothes with permethrin, and using natural killers like Wondercide, available at Amazon and Chewy.
In the past, tick exposure was a worry in the summer months. Now, ticks appear in early spring before the snow has melted here in Vermont.
Wear light-colored, permethrin-treated clothing when entering areas where you might be exposed to ticks, such as areas of high grass or leaf litter or wooded areas, which are common tick habitats. Wear long pants and long-sleeved shirts.
Apply tick repellent to exposed body areas. General insect repellents will not be effective. Some natural repellents and those containing DEET are the most effective, although not 100% effective.
Do a full-body tick check after coming indoors and remove your clothing outdoors.
Dry non-permethrin-treated clothing in the dryer for 5-10 minutes on high after removing them to kill any ticks on them. Take a shower, trying to wipe every inch of your body with a washcloth, then hit it with shower spray, and dry—again, trying to wipe every inch of your body by contact with the towel.
Learn about other types of ticks and tick-borne diseases. The lone star tick carries the bacterium that causes human ehrlichiosis. Other very serious illnesses are carried by ticks, such as the powassan virus and babesiosis.
BE SURE TO TREAT YOUR PETS FOR TICKS. My doctor told me that many humans are infected by ticks their pets carry into the house. You don’t even have to spend time outdoors or in high grass where you might encounter them.
Despite all this, it seems that tick bites are inevitable if you or your pets spend time outdoors. Be proactive and vigilant. But don’t let ticks stop you from enjoying the beauty of the outdoors.